Medical Directors in Home Health vs. Hospice Care: Roles & Differences
May 7th, 2025
5 min read
By Abigail Karl

When hiring for a home health or hospice agency, you may find yourself asking, “Do I really need a medical director? If so, what do they actually do?” A medical director’s role can vary significantly depending on the agency type. Home health medical directors have limited, mostly administrative duties. While hospice medical directors have central, hands-on oversight duties.
At the Home Health Consultant, we’ve processed hundreds of staff change applications. We’re well versed in the ins and outs of staffing regulations and want to help you feel ready to tackle hiring at your agency.
Table of Contents:
- Break down what a medical director does in both:
- Explain if and when medical director is required for both home health & hospice
- What qualifications medical director must have
- How the hospice moratorium affects medical director regulations
- What a CLIA waiver is and why it requires a medical director
- What is a PAC meeting & how it involves your medical director
- What to do if you need help finding a medical director
By the end of this article, you'll understand everything you need to know about medical directors, and steps to you need to take to ensure your agency is properly staffed.
What Is a Medical Director in Home Health and Hospice?
A medical director in both home health and hospice is a physician, but it’s a lot more complicated than that. Generally speaking, medical directors provide clinical oversight and ensure that care standards are being met. However, their level of involvement is incredibly different between home health and hospice.
Medical Director's Role in Home Health
In a home health agency, a medical director’s duties are usually limited to annual or semi-annual administrative tasks. These include:
- filling in for primary care physicians if a patient’s doctor is unavailable
- participating in annual or semi-annual policy reviews as part of the Professional Advisory Committee (PAC)
- helping the agency obtain and maintain a Clinical Laboratory Improvement Amendments (CLIA) waiver, allowing the agency to conduct and interpret basic lab tests
- acting as the CLIA medical director if the agency has a CLIA waiver
Medical Director's Role in Hospice
In Hospice Care, the medical director plays a crucial and active role in patient management. Their responsibilities include but are not limited to:
- developing and implementing patient care policies
- coordinating medical care to ensure patient comfort
- leading interdisciplinary group (IDG) meetings every two weeks
- certifying terminal illness and validating hospice eligibility
- ensuring compliance with federal and state regulations, as well as quality standards
- attending PAC meetings
- *in some cases, acting as the CLIA medical director
This comprehensive role makes the hospice medical director essential to both patient care and regulatory compliance.
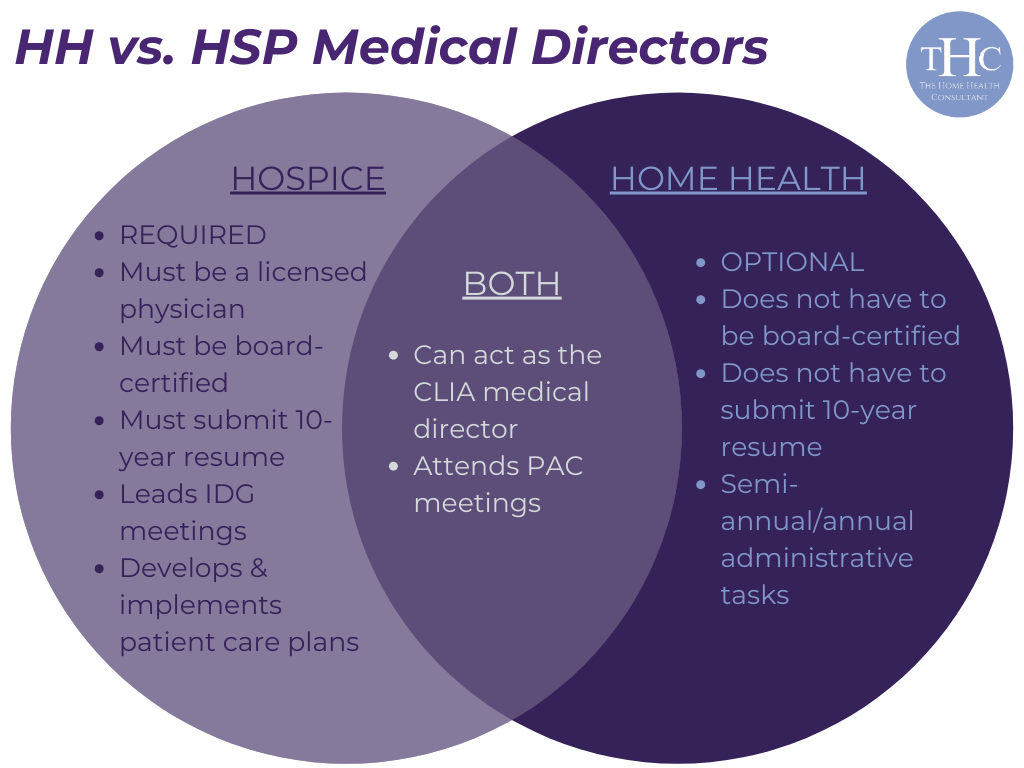
Is a Medical Director in Home Health & Hospice Required?
Home health and hospice agencies are similar in many ways, but a key difference is whether or not they require a medical director.
Is a Medical Director Required in Home Health?
For home health agencies, hiring a medical director is optional and generally not mandated by federal law or most state laws. In California, a home health Medical Director is not required.
Is a Medical Director Required in Hospice?
A hospice medical director is a required position and plays a crucial role in patient care and operational compliance. The roles differ so significantly because hospice care focuses more directly on end-of-life management. This demands consistent physician oversight to remain compliant with Medicare CoPs.
What Are the Qualifications for a Medical Director in Home Health vs. Hospice?
The qualifications for medical directors in hospice and home health differ significantly. This is due to hospice medical directors being required, and home health medical directors being optional.
Home Health Medical Director Qualifications
Home health medical directors are required to be a licensed physician (M.D. or D.O.). But, they are not required to be board-certified in any specific specialty or submit a 10-year resume.
CLIA Medical Director Qualifications
There are no federal requirements for a CLIA medical director overseeing waived tests. In California, however, a CLIA medical director overseeing waived tests must be a licensed physician. This requirement will vary depending on the state.
Hospice Medical Director Qualifications
To qualify as a medical director in hospice, applicants must be:
- A licensed physician (M.D. or D.O.)
- Able to Submit a 10-Year Resume to CDPH (for hospice only). In California, all key staff applicants must include all of the following information on their 10 year resume:
- The start and end dates of each job
- Each job title
- The name of each employer
- The address of each employer
Please note, the qualifications for hospice medical directors are changing within the next few years. Very soon, hospice medical directors in California must be board-certified, in internal medicine or a field related to palliative care. This is due to the currently ongoing hospice moratorium.
What is the Hospice Moratorium, and How Does It Affect Your Medical Director?
The California hospice moratorium, enacted in 2022, pauses the issuance of new hospice licenses until at least 2027. The moratorium aims to tackle systemic issues in hospice care. This includes raising medical director qualifications.
Under the moratorium, all hospice agencies are essentially in a grace period. This grace period allows non-hospice-certified medical directors to serve for now, though certification will eventually become mandatory.
There will also be no “grandfathering-in” of medical directors already working at agencies without certification. This soon-to-be requirement adds pressure for current hospice medical directors to obtain certification before the new requirements start being enforced.
What is a CLIA Waiver, and How Does It Involve a Medical Director?

A CLIA waiver allows home health or hospice agencies to interpret basic lab tests, like blood glucose, on-site. This ensures rapid results for immediate patient care. A licensed physician must serve as the CLIA medical director, overseeing the agency’s compliance with CLIA standards.
A CLIA medical director will approve which tests the agency administers and ensure that clinicians are trained to handle these tests. Although obtaining a CLIA waiver is not mandatory, it is very difficult to provide quality patient care without one. This is especially true for home health and hospice agencies that manage diabetic patients requiring frequent blood glucose monitoring.
To learn more about a CLIA waiver and why your agency may need one, check out our explainer on the topic below.
What is a PAC Meeting, and How Does It Involve a Medical Director?
The Professional Advisory Committee (PAC) meeting is not federally mandated, but it is required in certain states, such as California.
During these meetings, agency policies, patient care quality, and emergency protocols are reviewed. A medical director’s presence or input is needed to approve these guidelines and ensure the agency aligns with regulatory expectations.
In hospice, the medical director may attend to provide clinical insight, but any physician, even one not employed by your agency, could fulfill this role if your medical director is unavailable.
Is Hiring a Medical Director the Right Move for Your Agency?
To determine whether or not your agency needs to hire a medical director depends on a few factors. The two biggest factors are whether or not your agency wants to pursue a CLIA waiver, and whether or not you are a home health or a hospice.
Should You Hire a Home Health Medical Director?
For home health agencies, a medical director is not required. However, having a medical director can be beneficial, particularly if the agency is seeking a CLIA waiver or intends to participate in the PAC meetings required by certain states.
For larger agencies, hiring a part-time or hourly medical director to fulfill these administrative roles might be advantageous for operational efficiency. Smaller agencies, on the other hand, may find that the cost and complexity of hiring a medical director outweigh the benefits, given their limited resources in home health settings.
Should You Hire a Hospice Medical Director?
In hospice care, hiring a medical director is crucial and non-negotiable. Hospice agencies should prioritize hiring a medical director who is not only qualified but also experienced in end-of-life care. Given the impending certification requirements under the hospice moratorium, agencies should consider candidates who have or are willing to pursue additional qualifications as needed.
What If I Still Need Help Navigating How to Hire with a Medical Director?
If you’re still feeling overwhelmed by navigating the different regulations, responsibilities, and qualifications for medical directors in home health or hospice, you’re not alone. Understanding these roles can be complex, and having expert support can make all the difference.
Our team at The Home Health Consultant has processed hundreds of staff applications for both home health and hospice. We specialize in helping agencies like yours meet Medicare regulations and maintain compliance, both in staffing and beyond.
If you'd like to learn more about our services and how we help your agency maintain, overall compliance, check out our proven process below.
If you're ready for a helping hand, feel free to reach out and schedule a call with us. With the right resources and support, you’ll be well-equipped to decide if and how a medical director can benefit your agency’s goals.
*This article was written in consultation with Mariam Treystman and Kelly McCarthy.
*Disclaimer: The content provided in this article is not intended to be, nor should it be construed as, legal, financial, or professional advice. No consultant-client relationship is established by engaging with this content. You should seek the advice of a qualified attorney, financial advisor, or other professional regarding any legal or business matters. The consultant assumes no liability for any actions taken based on the information provided.





