What Happens If My Home Health or Hospice Agency Fails a Survey?
July 4th, 2025
6 min read
By Abigail Karl

Your home health (HH) or hospice agency (HSP) has been up and running for several years. Your staff are amazing. Your clinicians are frequently complimented on their bedside manner and professionalism. So by the time your triennial survey rolls around, you’re not concerned.
But then the surveyor arrives and starts pointing out deficiencies left and right. Your anxiety starts rising. At the end of the first day, the surveyor lists the issues they found...including a conditional deficiency. What? How could this happen?
Not only do you not understand what caused you to fail the survey, but now you have to figure out how to fix it. What are your next steps?
Failing a survey can be a daunting experience for any HH or HSP agency. It can have serious ramifications for operations, revenue, and reputation. Understanding how survey failures happen and what can be done to recover from them is critical to your agency’s success.
After years in the HH and HSP industry, we at The Home Health Consultant (THC) are experts in everything you need to know about avoiding survey failure.
In this article, we’ll explore:
- The different kinds of deficiencies
- Which deficiencies cause you to fail a survey
- What happens if you fail your re-survey (Dependent Survey)
- Whether or not agencies can recover from a failed survey
- The consequences of an immediate jeopardy situation
- Whether or not agencies can recover from an immediate jeopardy situation
- Best practices for preventing survey failure.
After reading, you’ll know how to address and prevent a survey failure.
What is a Survey?
A survey is an inspection conducted by governing agencies or a national accreditor to ensure that HH and HSP agencies are compliant with all applicable rules and regulations. The three national accreditors contracted by CMS and various state agencies to conduct surveys are:
- The Accreditation Commission for Health Care (ACHC)
- The Community Health Accreditation Partner (CHAP)
- The Joint Commission (TJC)
During a survey, a surveyor from your accreditor will visit your agency’s office and sometimes patients’ homes. These surveys assess various aspects of agency operations, from patient care delivery, to clinical documentation, and administrative records. This is done to ensure that agencies are compliant with federal and state regulations.
Surveys are typically unannounced and can take place every three years for renewal. In some cases, they can happen sooner with specific events like a Change of Ownership (CHOW) or Change of Location (CHOL).
The amount and severity of deficiencies found during a survey determines whether an agency has:
- remained compliant
- requires corrective action
- Or, will go down the provider termination path, potentially leading to shut down
What Are Conditions of Participation (CoPs)?
Before we dive into survey failure prevention, you first have to understand the main reason agencies fail surveys.
Conditions of Participation (CoPs) are the standards set by the Centers for Medicare & Medicaid Services (CMS) that HH and HSP agencies must meet to participate in the Medicare programs.
These standards cover patient care, administrative processes, and safety regulations. Compliance with CoPs is mandatory for HH and HSP agencies that want to treat and bill Medicare patients. Surveys are Medicare's way of making sure you're following these regulations. If you’re deficient in just one CoP, you fail your survey.
What are Deficiencies and the Kinds of Deficiencies?
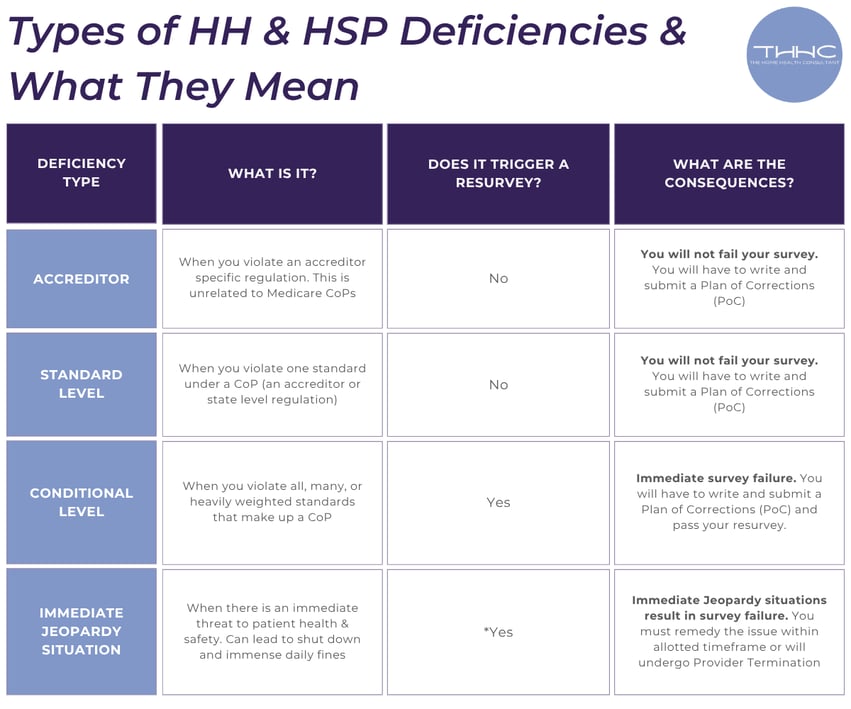
During a survey, deficiencies are areas where an agency falls short of meeting the regulations. Here are the different levels of deficiencies:
1. State-Level Deficiencies: occur when you are not following a regulation set by your state. In California, the governing body is California Department of Public Health (CDPH). Failure to meet state level regulations can result in loss of your license and ability to treat patients. For Medicare certified home health or hospice agencies, losing your state license automatically results in provider termination.
2. Accreditor-Level Deficiencies: occur when you are not following a regulation set by your accreditor (ACHC, TJC, or CHAP). Accreditor level deficiencies will not cause you to fail a survey.
3. Standard-Level Deficiencies: occur when you are not following a single, or very few, rules set by CMS.
You can think about Medicare regulations deficiencies like a Russian doll. A CoP is the biggest Russian doll. The standards underneath each CoP are the smaller dolls that sit inside the biggest doll. So, a set of standards define and make up a COP. Standard deficiencies are lower-level Medicare infractions that do not lead to failure or resurvey.

4. Condition-Level Deficiencies: occur when you're largely out of compliance. Again, each CoP is made up of numerous standards. A conditional level deficiency occurs if you have not met the majority of standards underneath a CoP. A conditional level deficiency can also occur if you have not met a heavily weighted standard underneath a CoP.
Conditional-Level Deficiencies are high level violations that lead to failure and resurvey. They signal that the agency is failing to meet one or more of the CoPs in a substantial, widespread way.

5. Immediate Jeopardy Situation: Immediate Jeopardy is the most critical deficiency. It represents an immediate threat to patient safety and results in survey failure, steep fines, and sometimes permanent shut down.
Which Deficiencies Cause You to Fail a Survey?
Each CoP consists of one or more standards. If an agency is not deficient in all standards under a given condition, it is not classified as a Conditional Deficiency. However, if an agency is deficient in every standard within a condition (which could range from one to several standards, depending on the condition), it results in a Conditional Deficiency.
An agency fails a survey if it receives a Condition-Level Deficiency. A failure at this level triggers additional actions such as submitting a Plan of Correction (PoC) and passing a Dependent Survey within 45 days. A Dependent Survey only focuses on the area(s) that caused the agency to fail the initial survey.
A Dependent Survey is usually shorter, only taking 2-3 hours over the course of one day. The agency is responsible for paying the cost of a Dependent Survey, which varies per accreditation organization. For ACHC, it typically costs around $5,000.
If the agency passes the Dependent Survey, it remains in operation and can continue billing Medicare for services. If it fails, further action will be required.
What Happens If You Fail a Dependent Survey?
Failing a Dependent Survey can lead to another round of corrective actions and yet another Dependent Survey. While it’s rare for an agency to fail multiple Dependent Surveys back to back, it is possible. If the agency fails again, the accreditor may conduct a new review process, potentially leading to a provider termination if the issues persist.
Again, the cost of a Dependent Survey is typically around $5,000, though this varies by accreditor. This is a significant cost for smaller agencies, which often struggle to maintain compliance with limited resources.
What you may have thought was a small issue, could escalate quickly and cost you a small fortune. Failure to correct issues after Dependent Surveys can lead to involuntary termination.
While involuntary termination doesn’t trigger a shutdown, it removes your ability to bill patients on Medicare, and may affect some private insurance contracts as well. This minimizes your patient pool by a significant amount. Involuntary termination also results in a ban from re-applying to the Medicare program for 2 years.
Can an Agency Recover from a Failed Survey?

Yes, agencies can recover from failing a survey. Focus on implementing actions based on the Plan of Correction and passing your Dependent Survey. After this, many agencies have regained compliance and continued operations. In some cases, agencies that failed multiple Dependent Surveys were able to recover after adjusting their processes.
What are the Consequences of an Immediate Jeopardy Situation?
Immediate Jeopardy (IJ) is the most severe type of deficiency and represents a direct threat to patient health and safety. If an agency is found to be in IJ, it must correct the situation immediately.
Oftentimes there is a monetary penalty placed on agencies found with an IJ, ranging from $500-$21,000 per day. Failure to resolve an IJ can result in immediate termination of Medicare billing privileges and potentially lead to agency closure.
Can an Agency Recover from an Immediate Jeopardy Situation?
While an Immediate Jeopardy situation is serious, agencies can recover if they address the situation quickly, submit a Plan of Correction that satisfies CMS and the accreditor, and pass a dependent survey within 23 days. However, the margin for error is much smaller in these cases, and failure to act swiftly can lead to permanent consequences.
How Can I Prevent Survey Failure?
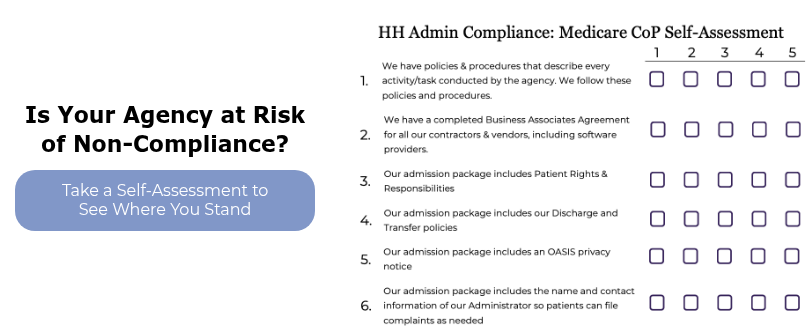
Preventing survey failure starts with understanding compliance with CoPs, the survey scoring system, and upholding processes for maintaining compliance. It’s a lot of information that you want to be sure you really understand before you find yourself in a sticky (and incredibly costly) situation.
The Home Health Consultant () helps agencies navigate the complex survey process and avoid failing by providing the following services:
- Survey Readiness: THHC assists agencies in staying ready for surveys, ensuring they understand what is required to meet CoPs and incorporate this into operations. We do this through our Administrative Compliance program.
- Direct Survey Support: THHC offers remote real-time survey support and assistance for our Administrative Compliance Program customers
- Plan of Correction Guidance: If an agency receives deficiencies, THHC helps develop and implement a PoC.
- Compliance Programs: The Home Health Consultant offers ongoing compliance programs to help agencies stay on track with evolving regulations.
With the right support and education, even agencies that have failed surveys can recover and get back on the path to compliance.
*This article was written in consultation with Mariam Treystman and Sarah Allen.
*Disclaimer: The content provided in this article is not intended to be, nor should it be construed as, legal, financial, or professional advice. No consultant-client relationship is established by engaging with this content. You should seek the advice of a qualified attorney, financial advisor, or other professional regarding any legal or business matters. The consultant assumes no liability for any actions taken based on the information provided.
Topics: