If you've ever found yourself second-guessing a signature on your home health or hospice documentation, you're not alone. This article will finally clear that up for good.
We’ve worked with countless agency owners, administrators, and QA professionals who’ve asked the same thing: “Do we need the time next to every signature? What if a signature is ineligible—is there a way to fix it?” With multiple accrediting bodies, vague CMS language, and inconsistent surveyor interpretations, it’s easy to feel like you’re walking a compliance tightrope.
At The Home Health Consultant, we’ve supported agencies through compliance and surveys for years. We’ve seen first-hand how something as small as a missing time stamp can snowball into larger issues like claim denials or deficiencies. The good news? When you know the rules and how to apply them correctly, you can avoid the pitfalls entirely.
In this article, we’ll break down:
- when timed signatures are required
- how rules differ between home health and hospice
- what to do if a signature is missing
- how to stay compliant with tools like signature logs and attestations
Whether you’re facing a survey, preparing for an audit, or just want to get your documentation tight, this guide will help you stay ahead of the game.
Are Home Health & Hospice Signatures Required to be Timed? It’s Complicated
Timed signature requirements vary slightly between home health & hospice agencies. For example, the CoP regarding clinical records in home health states:
“All entries must be legible, clear, complete, and appropriately
authenticated, dated, and timed.”
While there are no clear requirements for timing signatures, At The Home Health Consultant, we've noticed several surveyors from various accreditors did cite deficiencies for untimed signatures around 2020-2022. Perhaps through CMS clarification, this practice has since subsided.
Today, this CoP is interpreted as the timing of the interaction or service being performed. For example, the timing requirement is satisfied by documenting the start and end times of visits, case conferences and so on.
The CoP regarding orders in home health states:
“When services are provided on the basis of a physician or allowed practitioner's verbal orders, a nurse acting in accordance with state licensure requirements, or other qualified practitioner responsible for furnishing or supervising the ordered services, in accordance with state law and the HHA's policies, must document the orders in the patient's clinical record, and sign, date, and time the orders. Verbal orders must be authenticated and dated by the physician or allowed practitioner in accordance with applicable state laws and regulations, as well as the HHA's internal policies.”
Again, the current interpretation is that CMS requires the time of the interaction, not the act of signing the document. In the case of a verbal order, the agency must document the date and time the physician (or P.A.) verbally gave the order. The time of the actual signature for both the ordering clinician and the one receiving the order are not required.
On the other hand, the CoP regarding clinical records in hospice agencies states:
“All entries must be legible, clear, complete, and appropriately authenticated and dated. All entries must be signed, and the hospice must be able to authenticate each handwritten and electronic signature of a primary author who has reviewed and approved the entry.”
The hospice CoPs don’t mention timing as related to signatures of clinical entries. This does not mean that the time of the interaction is not required. Agencies must always indicate the time in and out of any visits.
While the CoP regarding orders in hospice agencies states:
“If a drug order is given verbally or electronically, it must be given to a licensed nurse, nurse practitioner, pharmacist, or physician, and must be recorded and signed immediately by the receiver. The prescribing individual must sign the order in accordance with State and Federal regulations.”
While the hospice CoP does not mention timing of verbal orders, at The Home Health Consultant, we encourage this as a best practice. Especially since the wording of the CoP does indicate some kind of time based nature with the word “immediately”. In this case, including the timing of the verbal order shows that the order was received and transcribed on the spot.
For both home health and hospice, the most common deficiencies we’ve seen cited for untimed signatures include those pertaining to:
- verbal orders
- electronic signatures (which need to capture the exact moment of signature for technical and universal compliance)
- clinical contractor signatures (PT, OT, ST)
While all signatures should be reviewed, pay extra attention to timing these areas. When in doubt, always be sure to check your agency’s policies and procedures, your accreditor standards, and the CoPs to ensure compliance.
Sometimes regulations are written vaguely, and enforcement is based on the interpretation of the government entity surveying you. For example, ACHC surveyors tend to interpret timed orders as noting the time of the interaction. Whether that’s the time the order was received verbally, or the time in and time out of the visit.
However, we’ve also seen TJC cite deficiencies if there’s no time of signature, which is different from time in and out. So again, it’s best to clarify how the governing authority surveying your agency interprets timed signature requirements.
Especially when CoPs are introduced or changed, it might take the community some time:
- to find interpretation gaps
- for CMS to make a determination on these interpretations
- to enact these interpretations into surveying and auditing guidelines
What to Do If A Signature is Missing on Medicare Home Health or Hospice Orders
Mistakes happen. A nurse might forget to sign a visit note, or a physician might fax back a plan of care without signature. What do you do if you realize a required signature is missing?
Medicare doesn’t allow “late signatures” beyond a reasonable short delay. In other words, you shouldn’t sign something weeks or months after the fact and pretend it was timely. You absolutely cannot pre-date or back-date an entry. That is considered falsification.
Also, Medicare will not accept retroactive orders. For example, a doctor cannot write an order for home health, after the care has been provided, and claim it was ordered properly. Orders need to be signed before or as care is provided, not well afterward.
However, there is a way to fix missing or inaccurate signatures. You can submit a signature attestation statement to Medicare. An attestation is a short letter or form in which the author confirms that a medical record entry is theirs, they have reviewed it, and approved it.
The attestation itself must:
- Be signed by the author
- Be dated by the author
- Identify the patient and record in question
Importantly, attestation is not allowed for orders. If an order wasn’t signed within the allowable window, Medicare’s stance is to disregard that order.
For example, an unsigned physician order for home health services means, in Medicare’s eyes, there was actually no valid order. You can’t fix this after the fact. Instead, you need to start from scratch with a new order. This delays your patient getting the care they need and can greatly affect your agency’s reputation. So it’s critical to get orders signed up front.
For other documentation, though, attestation can rescue you. Check if your Medicare Administrative Contractor (MAC) has a preferred attestation form or specific instructions. While not required, using their format can streamline review. And remember, the person who wrote the note must be the one attesting. You cannot have another staff member or physician sign an attestation on someone else’s behalf.
Below you’ll find a list of attestation statements for a few MACs. These are great examples to use if your MAC does not have a specific form.
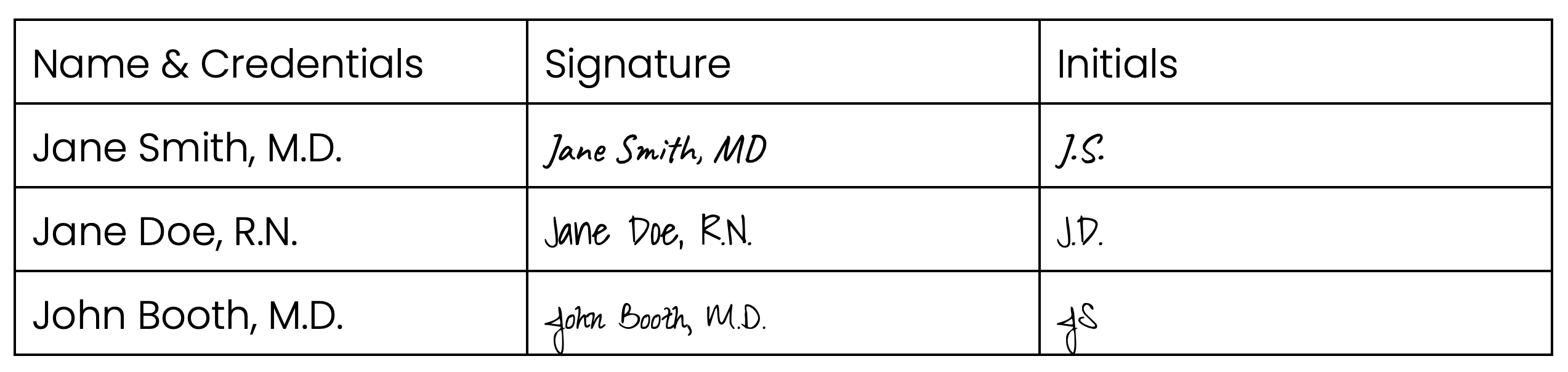
How To Fix Illegible Signatures on Medicare Documentation
Ever look at a doctor’s signature and think it looks like a scribble? Medicare reviewers sure have. If a signature is present but illegible, you need to provide evidence of who that signature belongs to. Otherwise, the reviewer might not know if the right person signed.
One easy solution is to ensure the printed name of the signer is somewhere on the document in addition to the signature. For example, many forms have a line like:
______________________
Dr. John Smith
If Dr. Smith’s signature is a scrawl, his printed name on the form can help connect the dots for the reviewer.
If names aren’t printed on the form, you can also use a signature log. A signature log is a typed or printed list of practitioner names with their corresponding handwritten signatures.
It can be an individual log (each clinician keeps one) or a group log for your agency. The log should also include the person’s credentials or title (MD, RN, PT, etc.). That way, if a first name/last name alone isn’t clear, the credential confirms the role. This ensures a claim isn’t denied simply because a reviewer couldn’t tell a physician’s qualification from the signature. Below you’ll find an example of what a signature log can look like.
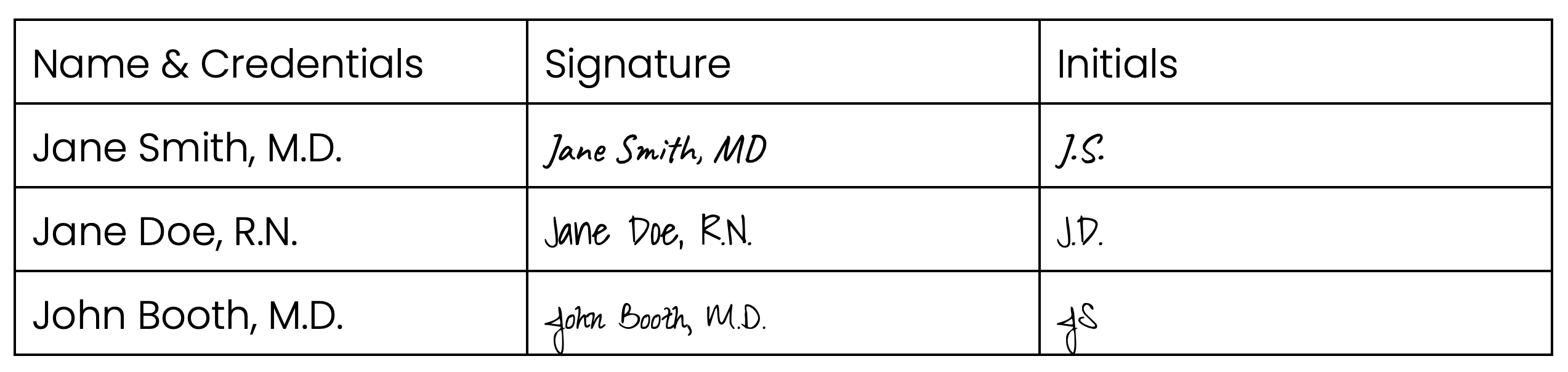
You can create a signature log at any time, even after the records are requested. Regardless, it’s smart to maintain signature logs proactively for all your clinicians. It’s a simple document to file away that could save your claim.
Pro Tip: If you know an order has messy signatures, consider automatically sending a signature log along with your records.
What ‘Special Scenarios’ Affect Medicare Signature Rules?
Medicare’s signature rules include some special scenarios that might apply in your agency:
- Using a scribe: Maybe a physician or nurse dictates while another staff member (scribe) writes the note. Medicare allows this, but the primary provider must sign the entry to authenticate it.
The scribe does not need to sign or date the note. Medicare doesn’t require a “scribe signature,” nor will it deny a claim because a scribe didn’t sign.
- Multiple-page documents: Home health or hospice plans of care can run several pages. Do you need a signature on every page? No, one signature can cover an entire multi-page document. Just make sure it’s clear that the pages belong together. Medicare recommends labeling pages like “Page 1 of 4, Page 2 of 4,” etc.
As long as all pages are properly numbered or linked, that single signature suffices to approve the whole content.
- Someone signing for someone else: Occasionally, an ordering physician might be unavailable. Can a different qualified doctor sign a plan of care? Absolutely not.
Medicare’s stance is that the one who orders the service must be the one who signs. A different physician cannot sign a certification or order if they were not the one who actually ordered the services.
For example, Dr. Lee gave a verbal order for home health, but Dr. Smith is covering the office this week. Dr. Smith cannot sign Dr. Lee’s order.
The only time another physician can sign orders is if they are taking over the care management of the patient. These cases must be documented in specific ways, with the new physician accepting to take care of the patient. If this is the situation you’re in, it’s not enough for the doctor to simply sign instead of the previous one.
In case you missed our breakdown of the basics, read our article: Medicare Signature Requirements for Home Health & Hospice (Part 1: The Basics) to get all the information you need to stay compliant.
When you follow these practices, you protect your revenue and your patients’ continuity of care. You’ll spend less time fighting denials and more time running your agency and caring for patients.