Emergency Vendors Medicare-Certified Home Health & Hospice Need
May 28th, 2025
4 min read
By Abigail Karl
If you'd like to listen to this article instead, our co-founder Mariam Treystman breaks it all down in the podcast below.
If an emergency hit your area today, could your agency keep delivering care?
Most home health and hospice administrators feel confident—until they realize Medicare emergency requirements go far beyond just a written plan. If you don’t have the right vendors ready to act, your agency is out of compliance, and worse, could be left scrambling to meet patient needs during a crisis.
*This article was written in consultation with Mariam Treystman.
At The Home Health Consultant, we work with agencies every day to strengthen their emergency preparedness programs and overall compliance.
Table of Contents
-
What Info Must Home Health & Hospice Agencies Collect from Emergency Vendors
-
What Are the 7 Essential Emergency Vendors for Home Health & Hospice Agencies
-
Why Emergency Vendors Are Essential to Compliance & Patient Safety
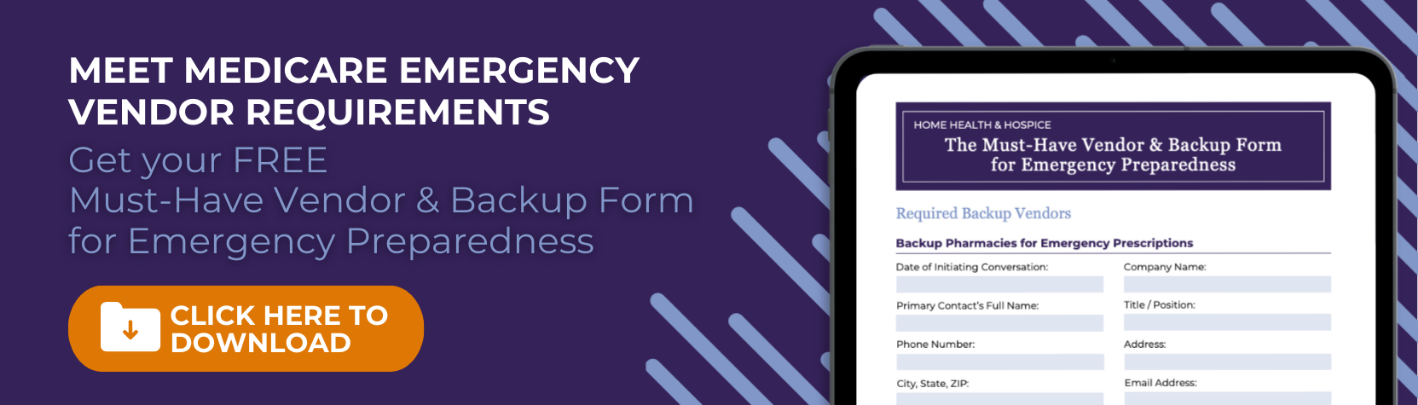
What Information Must Home Health & Hospice Agencies Collect from Emergency Vendors?
CMS and your accreditor (CHAP, ACHC, or Joint Commission) expect more than good intentions. Your emergency plan must include vendor agreements to maintain care continuity.
And these vendors can’t just be listed by name. You must document:
- Vendor name and company contact
- Phone number, address, and email
- Date of initial conversation or agreement
- Payment terms or arrangements
Each vendor agreement ensures you’re not left scrambling mid-crisis. You need backups who can act fast without waiting for contracts or billing approvals.
What Are the 7 Essential Emergency Vendors for Medicare Home Health & Hospice Agencies
There are seven main types of emergency vendors that CMS wants to see in your Emergency Preparedness Plan. We're going to explain each one below.
1. Backup Pharmacies for Emergency Prescriptions
If a patient’s regular pharmacy is inaccessible due to fire, flood, or evacuation, what’s your backup?
You need one (or more) pharmacies located outside your immediate area. These partners should be ready to:
- Quickly fill emergency prescriptions
- Accept your agency’s payment method on file
- Work off a physician’s order without delays
These don’t have to be formal contracts, but written agreements are best. Surveyors look for evidence that you’ve coordinated care continuity, not vague intentions.
2. Medical Supply Companies for Equipment Replacement
What happens if a patient evacuates and leaves their supplies behind?
This is one example (out of many) of why a secondary medical supply vendor may step in. Think walkers, wound supplies, grab bars, or hospital beds. You need someone to be able to replace your patients’ durable medical equipment (DME) if it’s damaged or lost in an emergency.
You’ll want vendors who:
- Can quickly deliver emergency supplies
- Understand home health or hospice needs
- Don’t require lengthy paperwork before acting
Again, this isn’t about locked-in pricing. It’s about having reliable partners in place ahead of time who can act quickly when needed.
3. Partner Agencies for Patient Transfers
Emergencies can disrupt operations or make your staff unreachable. That’s why your plan must include a trusted partner agency.
If you’re a home health, partner with another home health agency. If you’re a hospice, find a hospice counterpart.
These other agencies should be located outside your service zone and agree to:
- Temporarily take on your patients during emergencies
- Transfer patients back when your agency resumes operations
This is especially important during wildfires, floods, or mass evacuations when patient safety is at risk.
4. Non-Emergency Medical Transportation Providers
Not every patient can drive or has family nearby. In a crisis, you may need to help patients evacuate safely. A non-emergency transportation vendor ensures you can:
- Move patients out of danger zones
- Support those without caregivers or transportation
- Respond quickly without delay
You’ll want this vendor’s contact and payment info preloaded in your plan.
5. Emergency Medical Transportation and First Responders

Some situations are urgent and require clinical transport or rescue. In addition to non-emergency transportation, identify emergency transportation resources:
- Ambulance companies or mobile health services
- Local fire departments
Your fire department contact list should include:
- Station phone numbers
- Coverage areas
- Any mutual aid agreements
If access to a neighborhood is restricted during a disaster, your local fire department can help conduct welfare checks on patients where clinicians can’t.
6. Mental Health Therapists for Staff Crisis Support
Emergencies don’t just affect patients, they impact your staff too.
Having a licensed therapist or counselor on standby allows your agency to offer:
- One to two trauma support sessions for affected staff
- Post-incident debriefing for field teams
You’re not expected to offer long-term therapy, but this can go a long way in helping your team recover and return to service as soon as possible.
7. Emergency Shelters (Most Commonly TJC Specific)

If you’re accredited by The Joint Commission (TJC), you’re required to list shelters in your emergency plan.
Even if shelter details change during a disaster, TJC wants to see:
- At least one or two shelter options listed
- Pre-coordinated plans for safe evacuation
Shelters often pop up in schools, gyms, or stadiums during major events. Still, having a few “default” locations listed in your plan keeps you compliant and ready. We recommend taking this extra step whether you’re accredited with TJC or not for extra protection.
Why Home Health & Hospice Emergency Vendors Are Essential to Compliance & Patient Safety
Most vendors are happy to help, but only if they know what to expect. The key is preparation. Here’s a quick recap of what we covered in this article:
Here's a quick recap of what we covered in this article:
- Pharmacies
- Durable Medical Equipment (DME)
- Transportation (Both emergency & non-emergency)
- Patient Care Transfer
- Therapy
- Shelter
Would your agency pass survey today if a surveyor checked for this list? Could your agency act immediately if phones or power went out?
If the answer to either of these questions is no, or even maybe, you’re out of compliance and it’s time to update your emergency plan now.
Need Help Building or Reviewing Your Home Health or Hospice Agency’s Emergency Vendor Plan?
Need help creating or refining your plan? That’s what we do.
At The Home Health Consultant, we help agencies like yours build survey-ready emergency plans that actually work. Whether you’re preparing for CHAP, ACHC, or Joint Commission—we’ve got your back.
Want to make sure your emergency vendor list checks every box? Let’s talk. Schedule a call with us to see if we’re a good fit for your agency’s needs.
*Disclaimer: The content provided in this article is not intended to be, nor should it be construed as, legal, financial, or professional advice. No consultant-client relationship is established by engaging with this content. You should seek the advice of a qualified attorney, financial advisor, or other professional regarding any legal or business matters. The consultant assumes no liability for any actions taken based on the information provided.