Are you feeling anxious, confused, or even frustrated by Home Health Value-Based Purchasing (HHVBP)? As the 2025 rollout begins, many agency owners are grappling with uncertainty about what these changes mean for their operations, staff, and bottom line.
*This article was written in consultation with Mariam Treystman.
You might be wondering: Will my agency’s quality scores hold up? How do I ensure compliance without overwhelming my team? What happens if we fall behind? These are not just logistical questions—they’re pressing concerns that could shape the future of your agency.
At The Home Health Consultant, we bring over two decades of hands-on experience navigating regulatory shifts and optimizing agency performance.
We’ve broken down HHVBP in a clear, actionable way, so you can confidently adapt your operations. In this article, we’ll review:
By the end of this article, you'll have a solid understanding of how home health value based purchasing will affect your bottom line and next steps for protecting your payments.
What is Value Based Purchasing?
Home Health Value Based Purchasing (HHVBP) was a model first introduced in only nine states back in 2016. Now however, all Medicare certified home health agencies, in all fifty states, must follow the model. While HHVBP sounds incredibly complicated, at its core it’s just a system to help make reporting on Medicare Home Health patients’ data more clear and concise.
The goals of HHVBP are to improve patient care for those on Medicare, reflect on home health care quality and efficiency, and better the process for public reporting. HHVBP accomplishes this through multiple Quality Measures (QMs) Home Health agencies must report on.
When Did Value-Based Purchasing Start?
The nationwide rollout of HHVBP began on January 1, 2025, but CMS will use baseline data collected from 2023 to evaluate performance. Agencies’ performance in 2024, relative to the baseline, will determine payment adjustments for 2025.
For the quality measure Discharge to Community-Post Acute Care (DTC-PAC), CMS will reference both 2022 and 2023 data, as it requires a longer historical view to calculate standards.
What’s Changing for Value Based Purchasing in 2025?
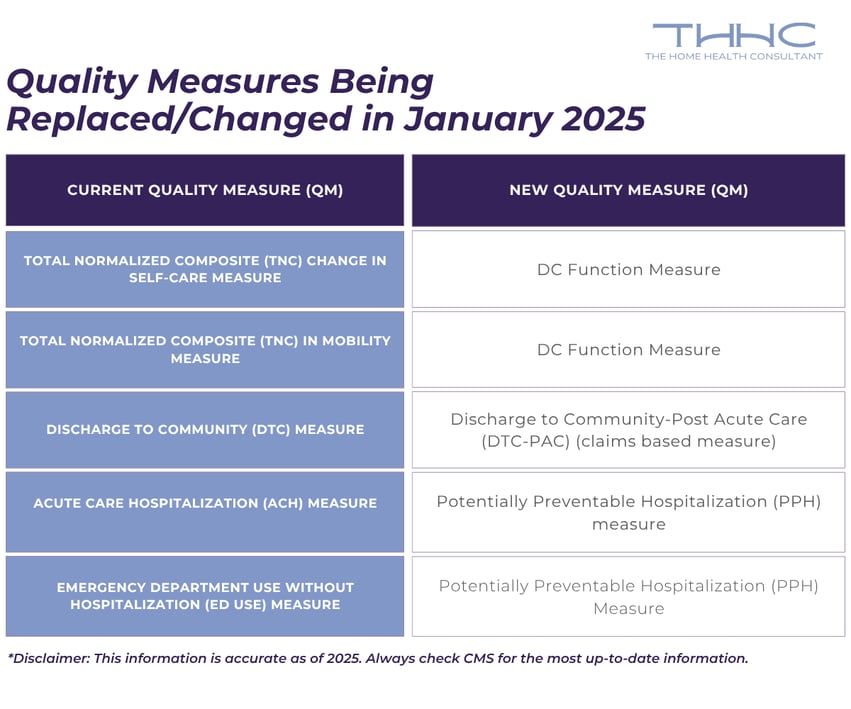
The main changes to Value Based Purchasing in 2025 concern Quality Measures (QMs). Quality Measures are tools used to evaluate different aspects of healthcare, like how well processes are working, patient outcomes, patient feedback, and how healthcare organizations are organized.
The Centers for Medicare and Medicaid Services (CMS) have their own quality measures (QMs) included in the Home Health Value Based Purchasing Model (HHVBP).
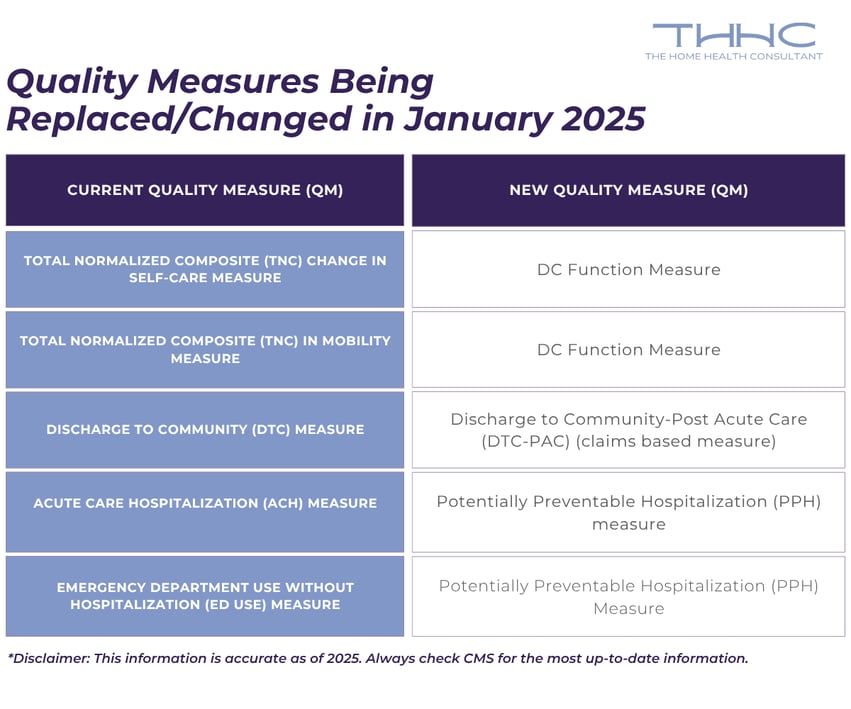
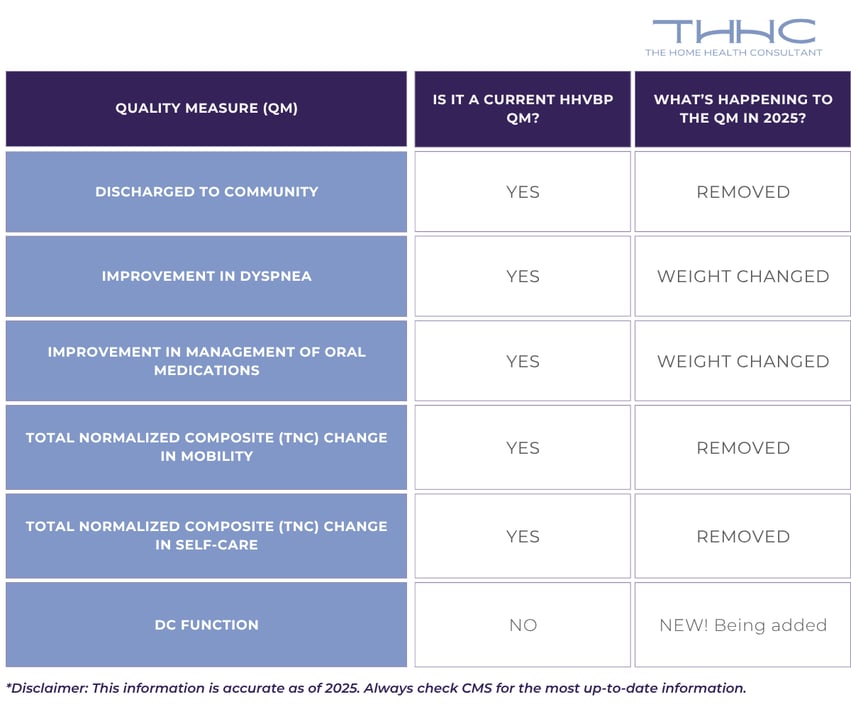
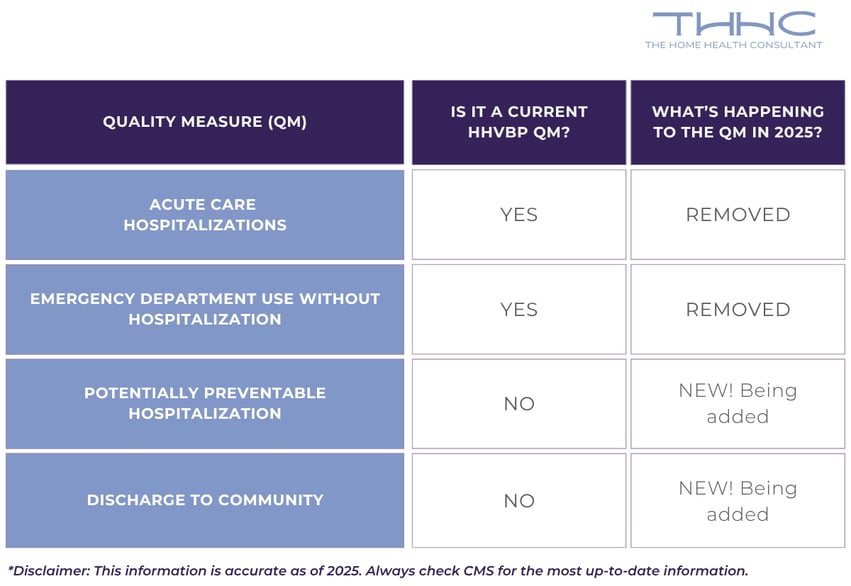
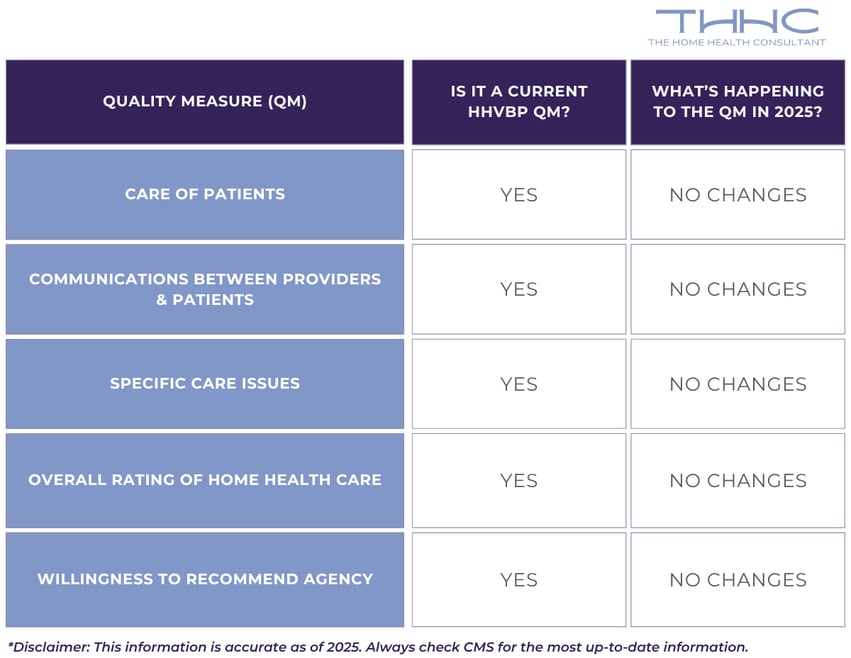
In the HHVBP updates being enacted in 2025, some quality measures have been altered or replaced. This is being done to improve the accuracy of the Home Health Quality Reporting Program (HH QRP). For home health agencies in states starting HHVBP this year, these measures will be completely new.
The chart below shows which current QMs will be replaced or changed starting in January of 2025.
The weighting system has changed based on the number of measures and cohort size.
Expanded Model Quality Measures
There are three different categories of quality measures (QMs), and each of these categories uses a different way to collect data. The three categories are Oasis-Based, Claims-Based, and Home Health Consumer Assessment of Healthcare Providers and Systems (HHCAHPS)-Based.
- Outcomes & Assessment Information Set (OASIS): The quality measures (QMs) are based on OASIS data that home health agencies (HHAs) collect and submit for all patients. As of July 1st, 2025 agencies must submit OASIS for *all patients, regardless of payor.
- Medicare fee-for-service (FFS) Claims: These are outcome measures used in the Home Health Quality Reporting Program (HH QRP) and are calculated using claims data submitted by home health agencies and other providers.
- Home Health Consumer Assessment of Healthcare Providers and Systems (HHCAHPS): The HHCAHPS survey collects feedback from patients about their home health care experience. The results include data from patients with Medicare and Medicaid, including Medicare Advantage and Medicaid managed care plans.
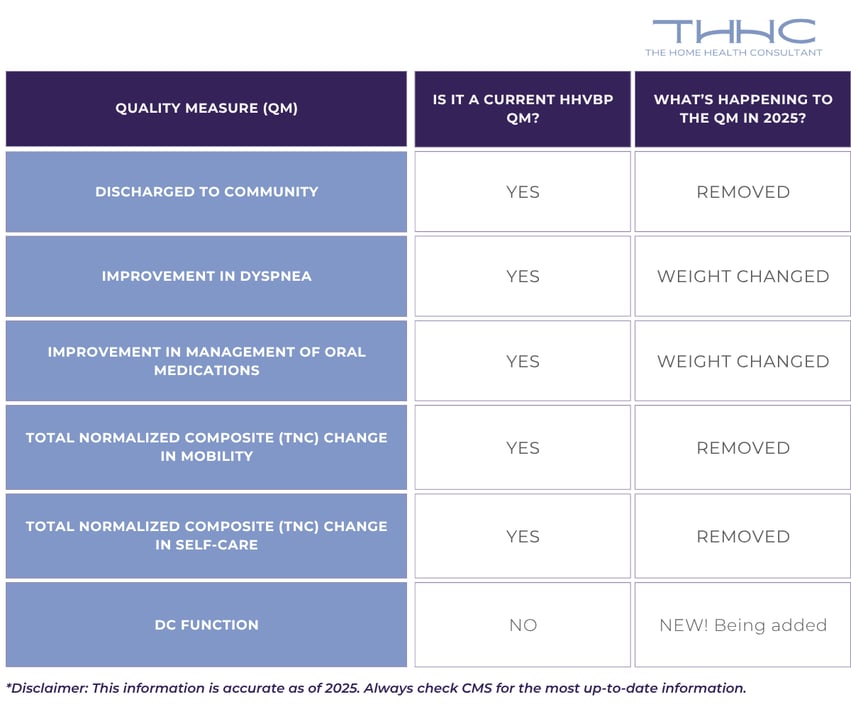
OASIS-Based Measures & Changes
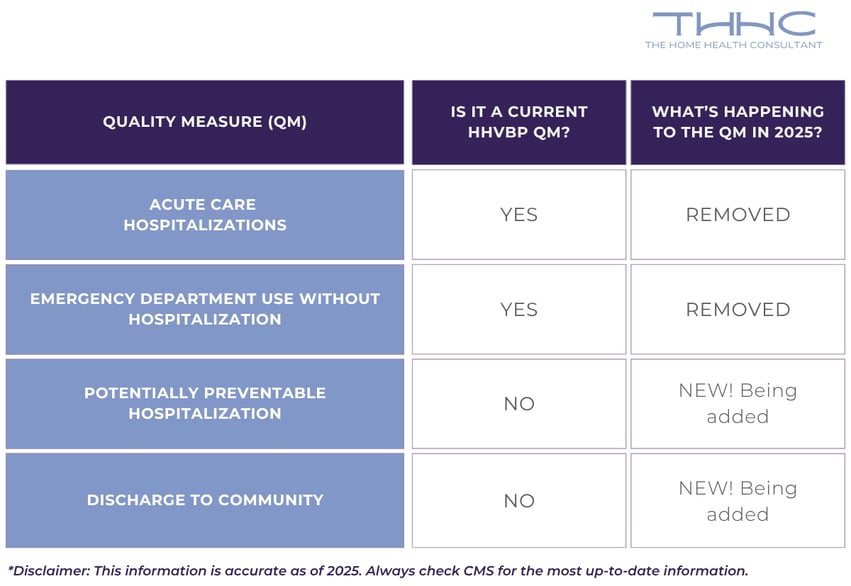
Claims-Based Measures & Changes
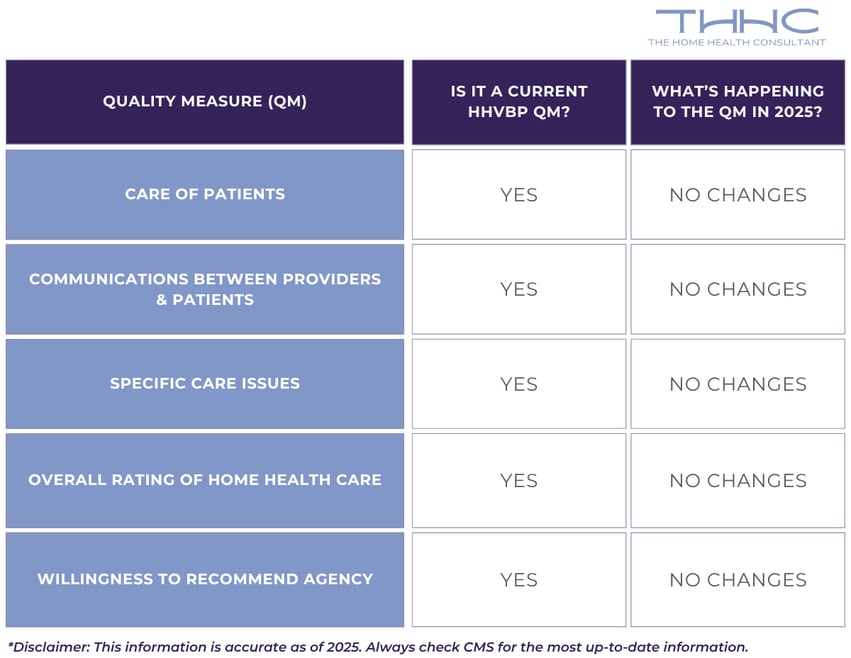
HHCAHPS-Based Measures & Changes
To learn more about the three QMs being added for 2025, CMS has additional resources and an in-depth training course available on their website.
How Will HHVBP Affect My Medicare Payments?
Under the Home Health Value-Based Purchasing (HHVBP) model, your Medicare payment will no longer rely solely on the patient's condition and the number of visits provided.
Instead, starting in 2025:
- 90% of your Medicare payment is determined by traditional factors like patient condition and services rendered
- 10% of your Medicare payment is tied to your agency’s quality and outcome scores
Agencies that outperform national quality benchmarks could see bonus payments of up to 5% above their claim amount. But, those performing below the average may face reductions of up to 5%. For example, if your agency typically bills $5 million annually, even a 5% bonus or reduction could equate to a $250,000 swing in revenue.
Maintaining or exceeding national standards will be critical. Late submissions of claims or failure to report required data, like HHCAHPS, OASIS, or claims, may result in additional penalties, impacting your quality scores. Agencies at the bottom tier of performance may struggle to remain operational in this competitive landscape.
At The Home Health Consultant, we’ve helped countless agencies navigate complex industry changes like this one. Our expertise lies in simplifying compliance, enhancing operational efficiency, and empowering agencies to achieve top-tier quality scores.